Renal Excretion of Metabolic Byproducts
How kidneys filter and eliminate water-soluble compounds from the body
Introduction to Renal Function
The kidneys filter the blood continuously, removing metabolic waste products, excess water, and electrolytes while preserving essential nutrients. Each day, the kidneys filter approximately 180 liters of blood plasma, ultimately producing 1-2 liters of urine. This massive filtration capacity exists to maintain homeostasis and eliminate compounds that would accumulate to toxic levels if retained.
Glomerular Filtration
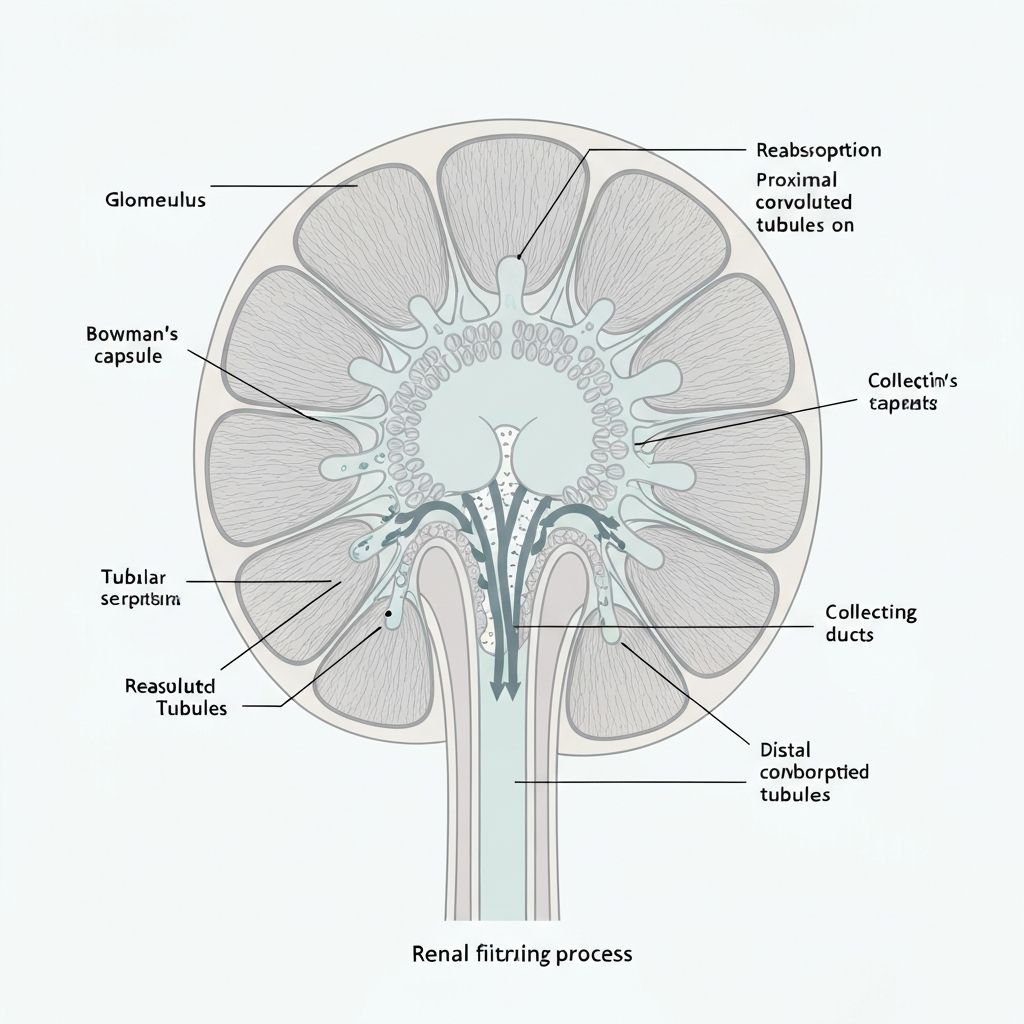
Glomerular filtration represents the first step of urine formation. In the renal corpuscle, blood flows through the glomerulus, a specialized capillary network, where hydrostatic pressure drives small molecular compounds across the glomerular filtration barrier into Bowman's capsule.
The Glomerular Filtration Barrier
The filtration barrier consists of three layers: the fenestrated endothelium, the basement membrane, and the podocytes. This barrier permits passage of small molecules (glucose, electrolytes, urea, creatinine) and water while preventing passage of large proteins and blood cells. The effective pore size is approximately 6-8 nanometers, allowing filtration of most molecules under 60 kilodaltons.
Hydrostatic Pressure Gradient
Net glomerular filtration pressure results from the balance between hydrostatic pressure in glomerular capillaries (approximately 60 mmHg) and oncotic pressure from plasma proteins (approximately 32 mmHg) opposing filtration. This pressure gradient, approximately 10-20 mmHg, drives continuous plasma filtration.
Tubular Reabsorption
Following glomerular filtration, the filtrate enters the proximal convoluted tubule where selective reabsorption occurs. Essential nutrients including glucose, amino acids, and electrolytes are reabsorbed via active transport and facilitated diffusion, returning to the bloodstream.
Proximal Tubule Reabsorption
The proximal tubule epithelium is specialized for reabsorption, with abundant mitochondria providing ATP for active transport. Approximately 99% of filtered glucose and amino acids are reabsorbed here through sodium-coupled cotransport mechanisms. Water follows osmotically, and approximately 65% of filtered water is reabsorbed in the proximal tubule.
Loop of Henle Concentration Mechanism
The loop of Henle creates osmotic gradients that enable concentration of urine and conservation of water. The descending limb is highly permeable to water, allowing passive water reabsorption. The ascending limb is impermeable to water but permits active reabsorption of sodium, potassium, and chloride through the Na+-K+-2Cl- cotransporter. This creates osmotic gradients in the renal medulla.
Collecting Duct Water Reabsorption
The collecting duct is where antidiuretic hormone (ADH/vasopressin) regulates water permeability. When ADH levels are high, aquaporin-2 water channels insert into the collecting duct epithelium, promoting water reabsorption and concentrating urine. This mechanism permits the body to conserve water during dehydration while excreting dilute urine when hydrated.
Tubular Secretion
Beyond passive filtration and reabsorption, the renal tubules actively secrete additional compounds from the blood into the filtrate. This active secretion handles metabolic waste products and xenobiotics that may not be efficiently filtered.
Secretion of Organic Compounds
Organic acids such as uric acid, creatinine, and hippuric acid are secreted in the proximal tubule via organic anion transporters (OAT) and organic cation transporters (OCT). This active secretion is crucial for eliminating metabolic waste including uric acid from purine metabolism and creatinine from muscle protein turnover.
Drug and Xenobiotic Secretion
Many pharmaceutical compounds and environmental contaminants are secreted by renal tubular transporters. This mechanism ensures efficient elimination of compounds that might otherwise accumulate systemically to toxic levels.
Urinary Concentration and Excretion
The final urine represents approximately 1% of the original glomerular filtrate. Its composition varies based on metabolic state, hydration status, and dietary intake. Normal urine contains water, urea, creatinine, uric acid, electrolytes, and trace amounts of other compounds.
Urea Excretion
Urea represents the primary nitrogen-containing waste product from protein metabolism. It is produced in the liver through the urea cycle and represents approximately 20-35 grams of daily nitrogen excretion in healthy adults. Urea is filtered at the glomerulus and partially reabsorbed in the collecting duct, allowing concentration of urine while maintaining osmotic balance.
Creatinine Excretion
Creatinine, produced from muscle creatine phosphate metabolism, is filtered by the glomerulus and minimally reabsorbed. Its constant production and renal excretion make it a useful marker of glomerular filtration rate (GFR). Elevated serum creatinine indicates reduced kidney function.
Integrated Kidney Function
The kidneys continuously filter, selectively reabsorb, and actively secrete compounds to maintain homeostasis. This process operates automatically and requires no external intervention or supplementation to function optimally in healthy individuals.
Related Articles
Liver Detoxification
Learn Phase I and Phase II pathwaysCommercial Products Evidence
Review clinical researchInformation Context
This educational content explains renal filtration and excretion physiology. It is provided for informational purposes only and does not constitute medical advice. For health-related questions, consult qualified healthcare professionals.